The Gold Coast Health and Knowledge Precinct’s inaugural Healthtech Summit showcased a future of profound hope – including for a life-changing spinal cord injury treatment and a high-tech solution for end-stage heart failure – in a healthcare system driven by personalised medicine and the power of AI to drive safer, better and more cost-effective healthcare.

Precinct Director Craig Rowsell kicked off the event in front of a full house at Cohort Innovation space, setting the tone for an afternoon of keynote speakers, fireside chats and an expert panel with a powerful and personal message: ‘health is everything’!
Perry Cross AM embodied that message, with his moving account of living with spinal cord injury (SCI) as a ventilated quadriplegic, and his inspirational quest for a cure for paralysis, including working with the original global champion of the cause, the late actor and Superman star Christopher Reeve.

Having doggedly navigated almost insurmountable barriers to be able to board a commercial flight to the US to meet the famous actor, Cross was then able to support Reeve, who’d suffered a similarly-severe SCI, to overcome the obstacles and secure his permission to fly.
Cross quipped: ‘my claim to fame is as the guy who taught Superman how to fly again’!
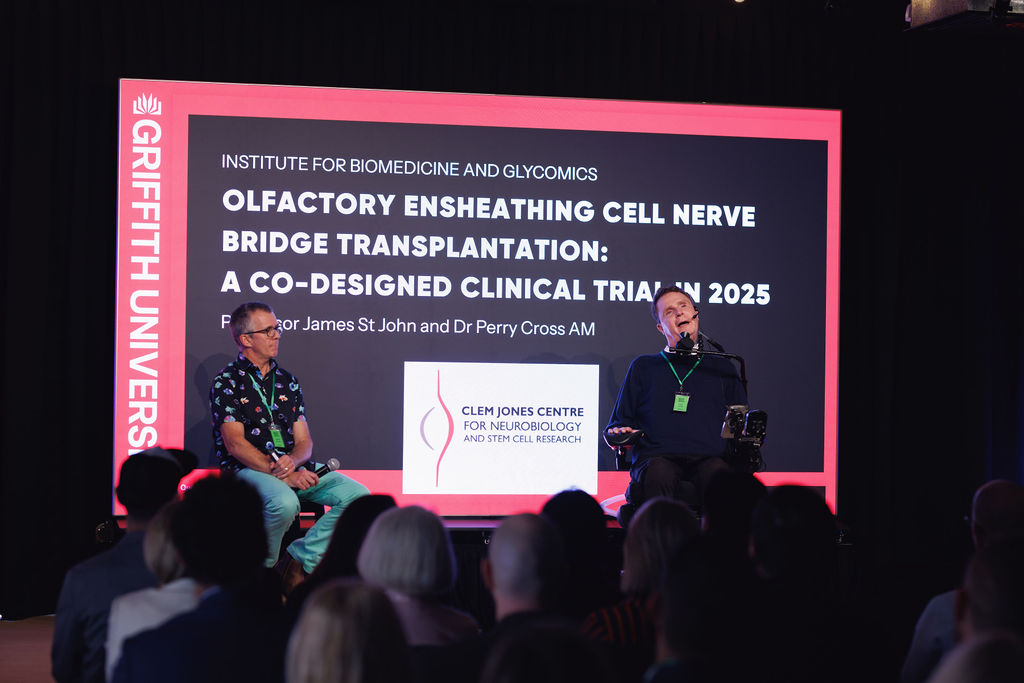
Griffith University’s Professor James St John then unpacked the science as he took over the story of their shared journey towards an SCI treatment that has culminated in a world-first novel cell transplantation therapy.

Having secured almost $40 million in research and clinical trial funding through grants and philanthropy over a decade, the pair, supported by a team numbering almost 300, are poised for the imminent start of a ground-breaking clinical trial.
Professor St John explained that their technology, which uses special cells harvested easily from the patient’s nose to create nerve bridges that guide neurons to repair the damaged spinal cord, had helped animals in studies regain mobility, sensation and autonomic function. Cell transplantation is paired with intensive exercise therapy to stimulate functional recovery.
While ‘walking again’ may be the focus in paralysis recovery, Professor St John outlined the many benefits they hope can be achieved: “from feeling cold and heat again to regulate temperature, to regaining bowel and bladder function and increased hand movement and dexterity for people living with quadriplegia – these are the critical improvements the SCI community really seeks,” he said.

The first fireside chat changed the tone but maintained hope, as Andrew Barnes, the Queensland founder of Edutech unicorn company G01, outlined how he created a ‘Netflix for Education’ that simplified professional learning across organisations large and small, supporting workplace training for over 50 million people globally.
In discussion with Cohort’s Dren Xërxa, Barnes, a Rhodes Scholar, spoke of being motivated to achieve impact through education, and of his shift to investing in healthtech, where the scale of impact can be even greater, but the innovation challenges are much harder.
According to Barnes, the right question makes all the difference – “I ask how can we do it? not ‘Can we do it?” and always question ‘Why Not?”. And in a nod to the merits of patience and persistence, he reflected on the growth of the GCHKP – “You don’t build ecosystems like this overnight.”

The second fireside chat provided ultimate evidence of the power of persistently questioning the ‘impossible’ and never flinching from the answer. BiVACOR‘s Geoff Tansley discussed the stunning success of clinical trials for their world-first rotary total artificial heart, developed by founder Dr Daniel Timms over a 20-plus-year journey of unflailing determination.
Dr Timms has been internationally lauded for his technology and tenacity, including making the cover of Forbes Magazine.

Conversing with the Precinct Office’s Kathy Kruger, Emeritus Professor Tansley, who is active in local mechanobiology research at Griffith University whilst leading global product development and heading up BiVACOR’s Australian office at Cohort, spoke of how trials in the US and Australia have gone even better than they’d hoped for.
The transformative device, which incorporates a single spinning disk that pumps blood to the lungs and body at different pressures while being magnetically levitated within the titanium heart to avoid mechanical wear, has now secured critical ‘Breakthrough Device’ status from the US FDA as a ‘bridge to transplant’. This smooths its eventual path to being the ultimate solution for end-stage heart failure.
Whilst Dr Timms had to move to the US for critical investment, Australia, and the Gold Coast, are positioned as key to current development and future plans: “We have a key Australian investor, significant funding as part of a $50m Medical Research Futures Fund (MRFF) for clinical translation, key talent and research partners, and we plan an R&D and APAC manufacturing hub right here,” Professor Tansley said.

Australian investors have been slow to target healthcare for transformation, according to an expert panel, led by Medtech executive Richard Nash.
The consensus: with the risk-averse healthcare sector lagging behind the AI-driven revolution taking place across other industries, challenges to innovation, including increasing venture capital, must be overcome to secure personalised and precision medicine that harnesses the power of AI.
VC investor and technology mentor Klaus Bartosch of Dreamoro spoke of replacing fear of AI with education to achieve ‘Medicine 3.0’, arguing investors want AI in their tech. Bartosch is a long-term mentor in Cohort’s LuminaX (LX) Healthech accelerator program.

Mani Sahihi, CEO of integrated communications company Foxo, argued Australia has the advantage of ‘high trust in our healthcare system’ that would drive innovation through behaviour change, and shared her big dream of ‘data interoperability across nations’.
Foxo is co-developing a secure communication platform with Gold Coast Health, which will curb repeat patient presentations to the emergency department by providing easy outpatient support.
According to Nash, surgical robotics (driven by AI), digital twins, increasing identification of new biomarkers and Quantum computing will all feature in a transformed healthcare system.

Rapid-fire pitches, by Cohort-based contract drug manufacturer Southern RNA on the exciting future of personalised cancer vaccines using RNA therapeutic platforms, and former LuminaX winner Your Track, represented by Professor Dianne Shanley, further energised the audience – Professor Shanley spoke of helping millions of children globally to access child development assessment and support, thanks in part to AI powering the scale of their solution.
And Dr Stephanie Chaoussis provided the last word on AI in healthcare, drawing on her experience working with companies including Cohort-based Datarwe and Panacea AI.
Networking kept the buzz going, with a showcase of local healthtech start-ups providing even more proof that transformation is already here!























